Psoriasis is a chronic, immune-mediated skin disease that causes red, itchy, scaly patches. It most commonly appears on the knees, elbows, trunk, soles of the feet, nails, and scalp. Psoriasis is more common than you think; a study shows that it affects around 2% of the world’s population.
Unfortunately, it is a lifelong, chronic disease with no definite cure so far. It usually goes through cycles, flaring up for a few weeks or months, then subsiding for a while or going into remission. The good news is that medical treatments are now available to help manage the symptoms and side effects of psoriasis. Moreover, patients can incorporate lifestyle habits and coping strategies to help them live better with psoriasis.
This article will shed the light on the signs and symptoms of psoriasis, the factors that trigger psoriasis, the side effects of psoriasis, and all the different available treatments to help patients with psoriasis. All the information that you need to know will be explained in detail in this article.
Symptoms of Psoriasis
Psoriasis signs and symptoms can vary from one person to another, depending on their medical conditions, lifestyle, and the type and severity of psoriasis. Common signs and symptoms of psoriasis in patients include:
- Red patches of skin are covered with thick, silvery scales on the scalp, hands, elbows, legs, feet, trunk, etc.
- Small scaling spots on limbs, especially in kids.
- Dry, cracked skin on the scalp or limbs that may bleed or itch
- Itching, burning, or soreness in the affected areas.
- Thickened, pitted, or ridged nails on fingers or toes.
- Swollen and stiff joints due to psoriasis.
Psoriasis patches can range from a few spots of dandruff-like scaling to major eruptions that cover large areas of a patient’s skin. The areas that are most commonly affected are usually the scalp, face, palms, lower back, elbows, knees, legs, and soles of the feet.
What Triggers Psoriasis?
Psoriasis is a sort of unpredictable disease that can be triggered by various factors, conditions, and lifestyles. Some of the triggers that cause psoriasis include:
- Cold, dry weather: It has been noted that climates that cause dry skin such as drier, colder weather can trigger psoriasis. In order for you to avoid that, try to spend some time in warm, sunny weather and high humidity places. Keeping a humidifier turned on in your room during winter can be helpful.
- Stress: Stress and anxiety are two of the main triggers that cause psoriasis flareups. Try to stay calm and relaxed. Whenever you are anxious about something, try to talk to someone you trust about it, it would help relieve your stress.
- Some medications: These include some ”beta-blocker” (b blocker) which are drugs used to treat high blood pressure and heart disease; lithium, a treatment for bipolar disorder and severe depressive disorder; and antimalarial; pills taken to treat malaria. If you have psoriasis and you are being treated for one of those diseases, let your doctor know immediately.
- Infections: Some infections including strep throat and tonsillitis can trigger a special kind of psoriasis outbreak. It looks like small drops that show up mainly on your torso and limbs. HIV infection can also make psoriasis flareups worse.
- Skin Injury: In some people, cuts, bruises, and burns can cause a psoriasis outbreak. Even tattoos and bug bites might trigger a new lesion. In order to avoid such breakouts, wear gloves or put on an extra layer of clothes.
- Alcohol: Drinking alcohol excessively may trigger or worsen symptoms and interfere with treatments. Combining certain psoriasis medications with alcohol can result in dangerous side effects.
- Smoking: Using tobacco or being around secondhand smoke raises your risk of getting psoriasis and makes existing conditions worse.
- Pregnancy: Psoriasis symptoms might become better or worse during pregnancy. Usually, pregnant women who suffer from psoriasis are advised not to take their medication because it could harm the baby.
- Hypocalcemia: Hypocalcemia occurs in patients with Psoriasis Vulgaris. Psoriasis might get worse due to reductions in ionized serum calcium concentrations resulting from hypocalcemia.
Psoriasis Side Effects
Psoriasis affects the skin, scalp, nails, and joints. Here is what you need to know about the side effects that affect different parts of the body:
- Skin manifestation
- Well-defined red lesions, with thick silvery scales all over the body, mostly on the elbows and knees, except for the face.
- It could affect palms, soles, and genitalia.
- Nails
- 80% of patients experience nail changes.
- It could affect one or all nails on fingers and toes.
- Fingers are more commonly involved than toes.
- Pitting, while strikes (leukonychia), yellow dots (oil drops), separation of the nail from the nail bed ( onycholysis), and red strikes ( splinter hemorrhages).
- Joints
- Single or multiple joints.
- Small or big joints.
- Simple swelling to complete destruction to the joint.
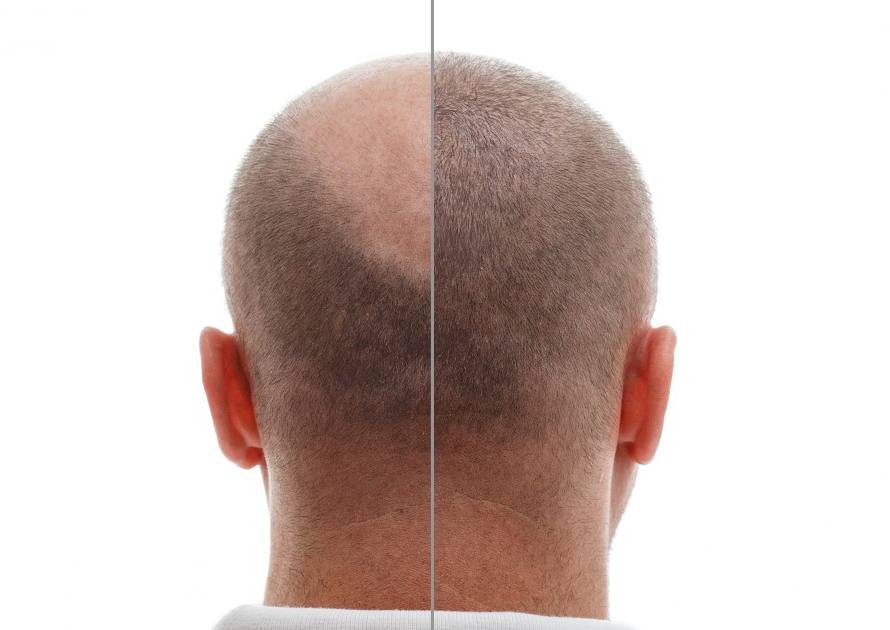
- Scalp
- Coarse dandruff.
- Red lesions on the scalp might over-follow the surrounding skin.
Treatment of Psoriasis
Psoriasis is a chronic disease that cannot be fully cured. However, there are treatments that can help patients cope with psoriasis and manage its sympoms and side effects. If your symptoms are particularly severe or not responding well to treatment, your general physican may refer you to a dermatologist.
Treatments are determined by the type and severity of your psoriasis, and the area of skin affected. Your dermatologist will probably start with a mild treatment, such as topical creams, or scalp lotions applied to the skin, and then move on to stronger treatments if your psoriasis does not respond.
A wide range of treatments are available for psoriasis, but finding the most effective one can be difficult. Talk to your dermatologist if you a treatment is not working for you or you have uncomfortable side effects.
Psoriasis treatments fall into 3 types:
- Topical: Creams and ointments applied to your skin.
- Phototherapy: Your skin is treated by exposure to certain types of ultraviolet light (UVA and UVB)
- Systemic: Oral and injected medications that work throughout the entire body.
Different types of treatment are often used in combination when necessary. Your treatment for psoriasis may need to be checked regularly. You might want to ask your dermatologist about the best tips for your daily life, and lifestyle.
Conclusion
Psoriasis is a lifelong, chronic skin disease that affects the scalp, hands, soles of feet, elbows, stomach, nails, etc. Psoriasis cannot be fully cured; however, psoriasis can be treated using different types of treatments including topical, phototherapy, and systemic.
You can manage psoriasis by changing lifestyle activities like eliminating smoking, drinking alcohol, exposure to cold and dry weather, and making sure that the medications you take are not triggering your psoriasis flareups.